With the seasonal changes that come with fall and winter, it is important to aid our immune systems to prevent catching any viral or bacterial infections that prevent us from enjoying all the holiday festivities!
How Did the Flu Become a Season?
Flu season, commonly known as the time of year when people are most likely to get sick from a strain of influenza. Like Summer and Winter, the flu “season” is known across all cultures. Imagine living in a completely different part of the world – would there be a flu season? After a quick online search, it is apparent the idea of a flu season exists in Europe, Asia, South America, and continents across the world. Does this global virus blow in with the cold winds of winter? How exactly does a virus come to have its own season? Let’s go back to the roots of this virus’s globolization.
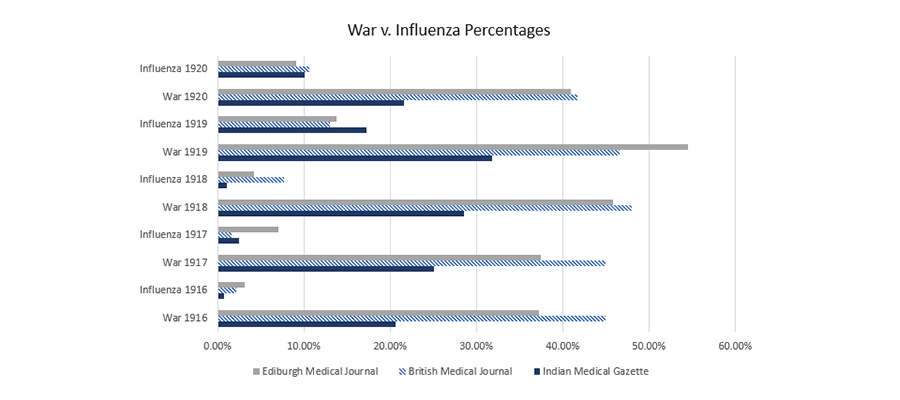
Right after World War I, the flu “pandemic” of 1918 spread across all countries involved and was first identified in the U.S. in soldiers after returning from the war. The virus traveled with military personnel from camp to camp and across the Atlantic, and at the height of the American military involvement in the war, September through November 1918, influenza and pneumonia sickened 20% to 40% of U.S. Army and Navy personnel (1).
While popular media called it the “Spanish Flu” that killed more than World War 1, this illness was not isolated to Spain and there is no reliable evidence to support these news headline claims. What we can deduce based on medical records is that vaccinated soldiers contracted the virus which most often led to a fatal pneumonia (2).
Alas, this viral infection is now present all around the globe and, like other viruses, can be spread by the coughing or sneezing of an infected person (3). But, people cough and sneeze year round – so, why does it appear that influenza is seasonal?
A common misconception is that the flu is caused by cold temperatures. Colder weather is not a cause, but a contributing factor to lifestyle. During the winter months, more time is spent indoors, less fresh foods are consumed, and there are more gatherings in close quarters.
A Season of Weakened Immunity
The shorter days of winter already result in less sunlight. This contributes to a decreased ability of the body to make pre-hormone “vitamin” D and melatonin. These low nutrient levels compromise our immune systems, which decreases our ability to fight infections.
Around the end of October, as the weather officially changes, so does the average diet. From Halloween to New Years, stress and consumption of sugar increase. This, combined with decreased sun exposure and outdoor activity, is a major factor in why the risk of being infected with influenza increases during the winter months.
This is good news! Because we are in control of our lifestyles, we can actually boost our immunity during these times and say good-bye to flu “season!” [/vc_column_text][vc_column_text]
How to Reduce Your Chances of Catching the Flu
When it comes to preventing illness, we can try our hardest to “avoid” coming into contact with viruses and bacterias and still fail. Most people encounter roughly 60,000 germs a day (3). Germs are actually a vital part of our immune system – they help keep it strong! Try thinking of these germs as your immune system’s workout regime. We don’t want to eliminate all germs – then our immune system would grow weak from never getting its “work out.” We also don’t want our immune system constantly working – can you imagine working out constantly and never getting a break? This is exhausting and doesn’t make us stronger at all! Strength happens with both exercise and REST. It is a beautiful balance our immune system must have to stay strong.
Don’t exhaust yourself trying to avoid germs. Rather, use common sense to keep a healthy balance of coming into contact with a variety of germs – exercising your immune system, and allowing your body to rest!
Supporting the Immune System
The best way to prevent getting sick and missing out on the joys of the fall & winter season is to support the immune system! This way, when the body is infected, it takes a shorter time to fight it rather than spending weeks feeling awful.
Crystal’s Tips for Supporting the Immune System:
1) Eat REAL Food
When we say real food, we mean food grown and consumed as it was designed – limiting over-processed, nutrient-stripped foods. Focus on eating whole plant foods grown in nutrient-rich soil that are grown in your local area!
In Cape Girardeau, our local farmer’s markets go into the fall months of October and November. When winter comes, we still have access to fresh, local foods grown by greenhouse farmers and sold at local markets or straight from the farm! Of course, if you can’t find local farmers or markets in your area, try to source organically grown whole foods from your closest super market. Organic doesn’t always equate to nutrient-rich, so be mindful. An organic toaster pastry is still a toaster pastry. Whole, REAL foods support the immune system with their nutrients, while processed foods weaken it (4).[/vc_column_text][vc_column_text]
2) Reduce GMO’s and Artificial Ingredients
When consuming more REAL foods, the intake of artificial ingredients naturally lessen. However, genetically modified organisms (GMO’s) are found in both processed foods and whole foods.
Genetic modification involves the transfer of genes from one species of plant or animal to another, using techniques that can cause mutations in the genome that may have unintended consequences for the crop’s safety. (5) The imprecise rearrangement of genes can create new proteins in these plants that may trigger allergies or promote disease. (6) Our immune systems often do not recognize these new proteins and may mount an immune attack against them if they enter our bloodstream intact.
These unintended gene transfers, along with those that are intended, can lead to significant changes in gut and immune function, and may have long-term consequences that are not yet known to the scientific and medical communities.
When it comes to food additives, there is accumulating evidence from nonhuman laboratory and human epidemiological studies suggesting that colorings, flavorings, and chemicals deliberately added to food during processing (direct food additives), and substances in food contact materials (including adhesives, dyes, coatings, paper, paperboard, plastic, and other polymers) that may come into contact with food as part of packaging or processing equipment but are not intended to be added directly to food (indirect food additives) may contribute to disease and disability in the population such as immune response (7).[/vc_column_text][vc_column_text]
3) Nourish the Body
When it comes to nourishing the body, add variety! A variety of movement, expression, active rest, and even a variety of foods. Unless we have in-depth testing done frequently, it’s hard to know what exactly our bodies need. However, if we consume a variety of nutrients through our food, then our body has access to whatever it may need!
Add variety through different meals, use different spices and herbs, try a new skill, read a book, enjoy a new essential oil, or go for a hike in a new place! Variety truly is the spice of life and it’s essential to nourishing the body!
4) Heal the Gut & Liver
We can eat all the nutrient-rich foods consumable, but it does us no good unless our bodies are able to absorb them. This is why it is SO important to heal the gut and the liver. Your gut’s influence over your health cannot be overstated. The trillions of microbes and colonies located in your microbiome are the manufacturers and managers of how you look, feel, and think. It makes up 70-80% of your immune system, produces a large amount of your “happy” neurotransmitter serotonin, and contains 10 times more bacterial cells than you have human cells!
The liver is always communicating with other digestive organs, receiving information about the level of available nutrients or the presence of threats like prescription medications, heavy metals or toxic substances. As the main organ involved in detoxification, it’s the liver that recognizes toxic substances and converts them into harmless material that can be released. As described in the World Journal of Hepatology in a 2017 article, “Beyond the metabolic functions, the liver recently has been defined as an organ of immune system (IS) … The liver keeps a delicate balance between hepatic screening of pathogenic antigens and immune tolerance to self-antigens.”
The gut barrier’s job is to allow nutrients out into the bloodstream while keeping pathogens and toxins safely locked inside the gut.When bad bacteria, LPS toxins, and other harmful compounds attack, they damage the gut barrier and escape into the bloodstream. From there, they can reach any part of your body and do even more harm.
The gut and liver do A LOT for us. Here are some things we can do for them:
- Reduce their burden through diet (ie. follow tips 1, 2 & 3)
- Follow Dr. Axe’s tips on liver health & gut health
- Schedule an appointment with Crystal or talk with your medical provider!
5) Support the Lymphatic System
The Lymphatic System is a critical part of the immune system, vital for protecting us from illness and damaging, disease-causing inflammation. Essentially, the lymphatic system is the the body’s inner “drainage system,” a network of blood vessels and lymph nodes that carry fluids from tissues around the body into the blood and vice versa.
The best way to protect the complex series of criss-crossing lymphatic vessels and “nodes” that span almost the entire body (every one except for the central nervous system) is to eat a healing diet (refer back to tips 1, 2, & 3), exercise and take steps to detoxify the body naturally such as massage, foam rolling, and infrared light therapy.
6) Get Outside and Enjoy Lots of Sunshine
Did you know that us Americans spend 90 percent of our lives indoors? Between commuting to and from our jobs, spending likely over eight hours a day working and going about our normal daily business, we see nature more on our TVs than we do in real life.
Not only is that a depressing statistic, but there are real health benefits of being outdoors that we’re missing out on when we’re confined to our homes and office buildings. Research suggests just 120 minutes (that’s two hours) per week is associated with good health and wellbeing. From improving our moods to feeling more relaxed, being outdoors is something we all could use more of.
Aim to spend 10–20 minutes of unexposed time in the sun daily (between 1,000 and 10,000 international units). The range is so wide as it depends on the time of year, how far from the equator you live and how much skin is exposed. If you have lighter skin, less time is needed. If you have darker skin or live farther north (in the Northern Hemisphere, like Boston), you need about an hour of sun in the summer to get about 1,000 IUs of vitamin D.
Struggling to figure out how you can add the health benefits of being outdoors into your lifestyle and spend more time outside? It’s not as difficult as you think.
Exercise outside. Take your yoga sessions to the backyard or skip the treadmill and visit the park instead.
Take a walk. Break up the mid-afternoon slump with a short walk outside, or go on a walk as you chat on the phone.
Eat outside. Enjoy a change of scenery and eat your meals outdoors.
Embrace seasonal activities. Cold outside? Play in the snow, head to the park or go for a brisk walk. Warm out? Try hiking or going to a swimming hole!
7) Laugh!
What’s one way you can hack your brain chemicals to boost your happiness? It’s as simple as laughing more.
Studies have found that people who laugh often benefit from stronger immune systems, more social support, boosts in their happiness and mood, diminished pain, protection against many diseases tied to stress, and even a longer, higher-quality life expectancy.
Not only does it feel good to laugh out loud, but it can lead to stronger friendships, and is even considered “natural medicine” for both your physical and mental health.[/vc_column_text][vc_column_text]
Acute Illness Items to Keep on Hand
Contrary to popular belief, a strong immune system does not mean never getting ill. We know how to limit our risk of viral infections and how to support our immune system, but what should we do when we do get ill? Continue to support the body with herbal remedies and supplements!
Crystal’s Recommendations:
Whole-food Vitamin C: Earthley Immune Aid, Pure Radiance, and Berry-C
P.S. Did you know we carry Earthley products in house!? If you’re in a pinch, call our office and hopefully we can share some of our inventory with you!
Make Your Own Fire Cider
Ingredients
- 1 medium organic onion, chopped
- 10 cloves of organic garlic, crushed or chopped
- 2 organic jalapeno peppers, chopped
- Zest and juice from 1 organic lemon
- 1/2 cup fresh grated organic ginger root (or organic ginger root powder)
- 1/2 cup fresh grated organic horseradish root (or organic horseradish powder)
- 1 Tbsp. organic turmeric powder
- 1/4 tsp. organic cayenne powder
- 2 Tbsp. of dried rosemary leaves
- organic apple cider vinegar
- 1/4 cup of raw, local honey, or to taste
Directions
- Prepare your roots, fruits, and herbs and place them in a quart-sized glass jar. If you’ve never grated fresh horseradish, be prepared for a powerful sinus-opening experience!
- Pour the apple cider vinegar in the jar until all of the ingredients are covered and the vinegar reaches the jar’s top.
- Use a piece of natural parchment paper under the lid to keep the vinegar from touching the metal, or a plastic lid if you have one. Shake well.
- Store in a dark, cool place for a month and remember to shake daily.
- After one month, use cheesecloth to strain out the pulp, pouring the vinegar into a clean jar. Be sure to squeeze as much of the liquidy goodness as you can from the pulp while straining.
- Next comes the honey. Add and stir until incorporated.
- Taste your cider and add more honey until you reach the desired sweetness.
Share Your Thoughts!
Have you tried any of these tips or recipes? We would love to hear from you! Share with us on social media or in the comments below!